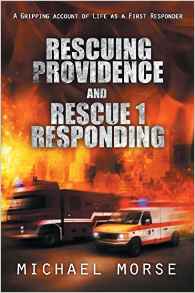
Rescuing Providence: Part 2 0530 Hours Through Part 3 0915 Hours, a Book by Michael Morse
Michael Morse, Author
Rescuing Providence: Part 2 0530 Hours Through Part 3 0915 Hours, a Book by Michael Morse
I’m glad I took the time to document what happens during a typical tour on an advanced life support rig in Rhode Island’s capitol city. Looking back, I can hardly believe I lived it. But I did, and now you can too. Many thanks to GoLocalProv.com for publishing the chapters of my books on a weekly basis from now until they are through. I hope that people come away from the experience with a better understanding of what their first responders do, who they are and how we do our best to hold it all together,
Enjoy the ride, and stay safe!
GET THE LATEST BREAKING NEWS HERE -- SIGN UP FOR GOLOCAL FREE DAILY EBLASTCaptain Michael Morse (ret.)
Providence Fire Department
The book is available at local bookstores and can be found HERE.
Note from the author:
Waking in the middle of the night, alone, with the very real fear that you are suffocating must be one of the worst experiences imaginable. Many of our elderly patients suffer from a condition known as CHF (congested heart failure.) As we age our heart can weaken and the part of it responsible for pumping oxygenated blood through our system, the left ventricle becomes too weak to do the job properly. Whatever it is that is happening in our body during an episode of CHF is translated by our brain into cognitive thought, and the message, “I AM GOING TO DIE!” comes through loud and clear.
One of the most gratifying calls any Paramedic or EMT can respond to is one where we can make a difference. Bringing a person the medications and interventions needed to get the oxygen levels back where they belong becomes business as usual to us, but for the people who depend on us, we are salvation.
Heady stuff for a simple firefighter…
0530 HOURS
CONGESTIVE HEART FAILURE
“Rescue 3, a still alarm.”
I am frozen in place, awakened by the familiar tone and covered in sweat, the sheets of my bunk a twisted wreck. My office is mercifully bathed in bright fluorescent light. I look around and see I am the only one there. I check my watch through blurry eyes, 0530. Sometimes it is better not to sleep during long shifts.
“Rescue 3 and Engine 12, respond to 534 Sandringham Avenue for an elderly female with difficulty breathing, history of CHF.”
I have responded to this type of emergency dozens of times since coming to rescue. Engine 12’s district is full of single-family homes with a large number of elderly residents. Rescue 3 responds to medical emergencies dealing with the elderly more than the other four trucks combined. There are 11 nursing homes or elderly high-rises in the district, so the potential for calls is enormous. Providence College is prominent in the area; the students and faculty mingle with long-term residents.
This time I have to wait for Renato to get to the truck. He makes it to the apparatus floor 30 seconds after I do, gets in, and starts the engine. Once again the overhead doors open, this time the first hint of light is evident as darkness grudgingly gives way to dawn. Sunrise is still an hour away, but a new day has begun.
“Do you know where we’re going?” I ask.
“Sandringham, it’s over by Engine 12,” he responds gruffly.
We both have bugs in our heads from lack of sleep. Renato puts his brain on automatic pilot and heads toward the Admiral Street Station, and I look for the street in the directory. Every truck has a street guide, and it comes in handy. Under normal circumstances, I would know exactly where the street is located. But my brain isn’t fully awake yet, so I need a little help from the book. Because the streets are deserted, we keep the sirens off during our ride. It makes no sense waking up the residents—the fewer people awake, the fewer chances of their calling 911. It is all about selfpreservation at this hour.\
In the five minutes it takes for us to get from Branch Avenue to Sandringham, I become fully awake. Engine 12 relays the message from the house:
“Engine 12 to fire alarm, advise rescue we have an 82-yearold female, conscious and alert, complaining of difficulty breathing. We’re getting vital signs now, but she is in obvious distress. History of CHF.”
“Rescue 3 received.”
The information from Engine 12 helped put my mind in gear. An elderly lady with trouble breathing, in obvious distress and a history of congestive heart failure is a serious situation. Her lungs are filling up with fluid because her left ventricle, the part of the heart responsible for pumping blood through the circulatory system, is weak and not able to keep the bodily fluid moving. As a result, her lungs are filling with fluid, and her airflow is diminished. Her blood pressure is probably skyrocketing and her pulse greatly increasing as her heart tries to compensate for the lack of powerful beats with rapid, weaker ones.
“Engine 12 to fire alarm, advise Rescue 3 her BP is 220/115 with a pulse of 120.”
“Rescue 3 received, on the scene.”
We pull in front of a beautifully kept colonial house. The front door is open and well lit.
“Get the chair,” I tell Renato as I make my way into the home. A set of stairs appears directly through the front doorway, and my patient is seated at the top in a small, wooden, armless chair surrounded by firefighters. An oxygen mask is over her nose and mouth, helping her breathe. Panic is evident on her face as we make eye contact on my way up the stairs. Renato is right behind me with the stair chair. The woman’s daughter is a few feet down the hall attempting to reassure her mom that everything will be all right. The crew of Engine 12 knows exactly what needs to be done and waste no time doing it. I give what I hope is a comforting squeeze to the patient’s shoulder as I pass, telling her not to worry and to hang on, that we will help her breathe. The guys are transferring the woman from her chair to ours while I talk to the daughter and get a history.
“She started having a little trouble last night, but it seemed to go away; then this morning she really started having trouble so we called you. She’s really getting worse. Is she going to be OK?”
“Has she ever had trouble like this before?” I ask.
“Last year she was in the hospital for two weeks after having a heart attack. The doctor has her on all kinds of medicine.” “What medicine is she on?” I ask.
“They know at the hospital. Let’s go.”
“I need to know. Do you have a list?”
“Just get her to the hospital,” she insists, obviously irritated by my questions. Beyond the woman I see seven or eight prescription bottles on a dresser in a bedroom.
“Are those hers?”
“For God’s sake, yes,” she answers, now in a panic.
I walk past her and scoop up the bottles. We carry the patient to the bottom of the stairs and to the back of the rescue, where the firefighters are preparing to move her from the stair chair to the stretcher. I enter the rig through the side door and get the truck ready. The first thing I do is turn on the O2. The portable tank that the engine company has her hooked up to is running low. Next, I turn on the EKG machine and get the leads ready. I move the IV kit to the bench seat as the stretcher is being rolled in. The patient looks worse, now gasping for air. Her lungs are full; immediate treatment is imperative.
All the guys on Engine 12 have extensive rescue experience. I pass the EKG leads to Tim, who places them in the right spots, and ask Renato to start an IV. Trial under fire. One of the other guys has hooked the patient to the pulsox and blood pressure monitor. I learn from the prescription bottles that the victim’s name isDolores. Her pulsox reading is 82 percent and her BP 240/130. While Renato starts the IV, I ask Tim to give her a nitro tab. Nitroglycerine is used to dilate the arteries and help with blood flow. Tim slips a 1/150 dose under Dolores’ tongue, and I tell her to let it melt and then give her a nebulizer treatment. Albuterol is placed in a reservoir, and O2 is added at approximately 6 liters per minute, which creates a medicated mist that dilates the bronchi. Renato wipes sweat from his forehead and informs me that the IV is ready. I look through Dolores’ medications and find what I am looking for. She takes a medication called furosemide, which is a diuretic used to adsorb excess liquid. Her dose is 40 milligrams a day. Our protocols call for us to double the amount during a breathing emergency and administer it through an IV. I draw up 80 milligrams, pinch the IV line, slowly push the drug through, and then flush with normal saline.
In a few moments I will reassess her vital signs to see if our ministrations have been effective. In the meantime, the look of relief on Dolores’ face tells me all I need to know. The stress level decreasing in the back of the truck is like the air being let out of a balloon that was ready to burst. We recheck her vitals, now 160/100 with a pulse of 100 and a pulsox of 92 percent. Not great, but a lot better than it was. The most important vital sign is Dolores’ face. She has relaxed now, relief flooding through her eyes in the form of tears, and her breathing has returned to normal. Renato looks as though he has just witnessed a miracle. How anybody could think that what we do is ordinary is beyond me, I think, as I wipe the signs of my own relief from my face.
One of the firefighters from Engine 12 drives the rescue over to Our Lady of Fatima, which is the closest hospital, and the Engine follows. Dolores’ daughter sits on the bench seat and keeps an eye on her mom as we make our way to the ER. I observe Renato’s reaction as we drive. It is obvious he is reveling in the beautiful feeling you get when you save somebody’s life. Dolores would have been dead minutes ago if not for our intervention. Renato knows it, yet he can’t believe what he has just done. I think I may have found a replacement for Mike.
I fill out the report while monitoring Dolores’ vital signs, the facts of what we just accomplished filling the empty paper but never able to tell the whole story.
PART 3
RESCUE LOG, LIEUTENANT MORSE
THURSDAY, 0800 HOURS
I have 10 hours to go. All things considered, it hasn’t been a bad night. A few hours of sleep go a long way, and I can see the light at the end of the tunnel. Unfortunately, sometimes that light is a train coming at you full speed ahead.
Dolores is in good hands. Her condition was greatly improved from the time we arrived at her house until she was admitted. I can barely contain Renato’s excitement as we drive back to the station. “What a night,” he remarks, still full of adrenaline. “I love Ladder 4, but tonight was unbelievable! We saved that old lady’s life! And the kid who got shot! I helped more people tonight than I have since I got hired!”
Renato has learned a lot and is making a good name for himself department wide, but his first night on a rescue is a real eyeopener. I hope he is hooked. Renato and I leave together. He is tired but still beaming from the night’s events. I have to get back to Rescue 1 and relieve Mark, who is in charge of the rescue on B Group.
“Let me know if you ever need a partner,” he says, which is music to my ears.
“I just might,” I tell him, trying not to get too enthusiastic. When the rush wears off after a night like we just had, people sometimes come to their senses and decide they are happier fighting fires, although those fires are becoming few and far between.
We shake hands at the bottom of the stairs. Renato starts his Lexus, and I crank up the old Toyota. I was seriously considering leaving the rescue division after Mike left. Training a new partner is hard enough, but it is torture training somebody who would rather be somewhere else. Most of the people who get sent to rescue put their best foot forward and do their best, but their heart is not in it. Renato seems to truly enjoy the work and isn’t adversely affected by the volume of calls. I will keep my fingers crossed. If I leave rescue, I will lose the overtime and have to get a part-time job. The cleaning business is an option, but I had hoped to retire my mop. Time will tell. For now I take it day by day and hope things will work out. Not a foolproof plan, but it’s the only one I have.
Traffic is light, and I am back in Rescue 1’s office 10 minutes later.
Mark is lying in the bunk with one eye open, “ready wrapped,” a firefighter term for somebody who sleeps with his clothes on.
“How was your night?” he asks. I tell him about the shooting. He has already heard most of the story from the people at the ER, but rescue guys like to share the details that nobody else hears.
“This city is nuts,” he says, shaking his head as he picks up his things and gets ready to head home. His night was also busy, “four after,” another firefighter term for the number of calls that you have between midnight and shift change.
My energy is holding up, but I have a long way to go. Weekdays are brutally busy. As the city’s residents are joined by thousands of workers from out of town, the potential for medical emergencies increases immensely. I know I’ll be running all day with little hope for a break.
“No time like the present,” I say to the empty office, slipping into the bunk, still warm from Mark’s body heat. Kind of gross, but at the time I don’t care. Mark gives me the radio and leaves. I am sound asleep in minutes.
0915 Hours
ALLERGIC REACTION

Here we go.
“Rescue 1 and Engine 9; respond to the Steere House for a possible allergic reaction.”
I fumbled for my radio and say, “Rescue 1 is on the way.”
Mike is back in the driver’s seat, looking refreshed.
“You look like shit,” he says.
“Thank you,” I reply, “and fuck you.” His laugh fills the small space, infecting me. I am going to miss him.
We leave the station, lights activated and siren wailing, quickly making our way as the other vehicles move to the side of the road. The Steere House is a nursing home located about five miles from the station, right around the corner from Rhode Island Hospital.
I used to think that I wanted to live forever. If I couldn’t live forever, I thought 100 years would do. Now that I have seen how so many of our elderly citizens spend their last few years on earth, I have decided that, if at all possible, I want to die with my boots on. I realize that there are not many alternatives to nursing home care at the end of our years, but I hate to see a person’s dignity fade at the end of a long, productive life.
My mother lives in a nursing home after suffering a massive stroke in 1996. Her care is the best available, much better than my siblings or I could provide in our homes. Sadly, something is sorely lacking. The elderly once had a position of honor in our society, earned through a life of accomplishment. Now they sit or lie in their beds, heavily medicated revenue-producers for nursing home owners. Their days end in a sterile environment full of strangers, waiting and hoping in vain for somebody from their past to visit. As time progresses, the staff members at the homes become more important than their families. When I can, I stop by the nursing home. My job and the odd hours I work afford me the luxury of stopping by whenever it is convenient. Sometimes that is at 2:00 in the afternoon, in the middle of visiting hours when everybody is on their toes; other times I’ll drop in at 2:00 in the morning, surprising the night shift. They have never given me a reason to worry about the care my mother receives.
After the stroke she was feisty, even insisting that she be brought home. I thought she had a chance. Instead, her body wore down as time progressed. Her personality slowly disappeared, receding into the shell of her withering body, and she was unable to communicate. Visiting her feels like I’ve taken my heart out of my chest, squeezed the life out of it like a spent dishrag, and then thrown it on the floor. I’ll sit for a while; she’ll look at me with eyes full of intelligence that she can no longer share as I wait for the next call. Sometimes it is fast, and I begin the healing process quickly. Other times an eternity passes before somebody else needs me and my radio breaks the silence in the room. At those times I long for anything to get me out of there. I’ll give her hand a squeeze, kiss her on the forehead, and then walk away. My heart eventually returns to normal, but I think I leave a little on the floor every time I visit. I can only imagine how my mother feels.
The nursing home is filled with characters. I wonder why some of the elderly maintain a lively, optimistic spark while others are filled with resentment. We all lead similar lives; our hearts get broken and then mended again and again, at times hurting so badly it seems death may be preferable to life. I wonder whether the resentful have had their hearts broken so often that their hearts become filled with shattered pieces, leaving no more room for pain, while those with more optimism escape the brunt of the heartache that most of us bear. Perhaps some are able to deal with grief more efficiently than others, storing the shreds of crushed dreams, lost loves, and failing health someplace they stay forever buried.
I place the blue canvas med bag on the stretcher, and Mike and I work our way through the front doors of the facility and into the lobby. Inside the canvas bag is everything needed for handling an onscene emergency: an IV setup, all the drugs we are licensed to carry, intubation equipment, a bag/valve device, and trauma dressings.
A grand piano, beautiful floral arrangements, sofas, and chairs fill the lobby. A big, yellow alley cat sleeps on the grand piano. I rub the top of its head on my way past; it is asleep and barely stirs. “Engine 9 to fire alarm, advise rescue we have a 25-year-old female, possible allergic reaction.”
“Rescue 1 received,” I say into the mike.
I think I heard Pat, the officer of Engine 9, say a 25-year-old, but I am sure he is mistaken. Ninety-five is the age of most of our patients here.
The guys from Engine 9 are on the second floor, so we head to the elevator, push the right buttons, and begin our ascent. The door opens to three firefighters hovering over a person lying on her back in the hallway, covered with a sheet. I am impressed with our guys’ dedication and efficiency. They are doing everything possible to make the patient more comfortable: monitoring vital signs, giving supplemental oxygen, and treating her with the utmost kindness and care. I can’t recall seeing this much enthusiasm for a patient since the last time we went to the Foxy Lady to treat a dancer who had fainted. The closer to the patient I get, the clearer the situation becomes. She is indeed 25, beautiful, and covered with hives, but she is breathing normally. She is embarrassed by all the attention.
“What happened?” I ask her after fighting my way through the firefighters.
“I took some new medication this morning, an antibiotic,” she explains. “When I got to work, I began to itch all over. Then I noticed these hives.”
Red bumps and welts appear on her face and arms, probably under her clothes as well. I hope there are no hives internally. She looks as though she spent the night in a jungle without a mosquito net. I scratch an imaginary itch on my arm.
“Are you having trouble breathing?” I ask.
“No, but I am really itchy.”
“We’re going to take you to the hospital so they can check you out,” I tell her while scratching my head.
“Do I have to go? I think I’ll be fine in a little while.”
“I think you might start to have trouble breathing. If your airway swells up, you could be in a lot of trouble.”
She recognizes the situation as potentially serious and acquiesces. “All right, let’s go,” she agrees reluctantly.
She tries to talk us into letting her walk, but we insist on putting her on the stretcher. The elderly residents get a kick out of seeing one of their caregivers on their end of things, even if only for a little while. I’m only too happy to give them a little entertainment.
The guys from Engine 9 help us get the patient, Sarah, into the truck.
“Thanks for the help, guys. We’ll take it from here,” I say.
“Anytime,” Pat replies.
“Take care, Sarah,” says Ben, grinning from ear to ear. “If you ever need anything, you know who to call.”
“You guys have been great,” responds Sarah as I close the rear doors of the rescue. The firefighters reluctantly go back to the engine, their job well done. Mike and I have some work to do before transporting.
“Quit scratching yourself,” orders Mike. “It’s only a subliminal suggestion.”
“I’m not scratching,” I say, taking the tip of my finger out of the ear I was scratching. If somebody starts to yawn, I’ll be in big trouble.
“We’re going to give you some oxygen and an IV just to be safe,” I tell Sarah.
“Is all this necessary?”
“Why are nurses always the worst patients?” I ask her.
With a knowing conspiratorial look, she replies, “No worse than firemen.”
Mike hooks her up to the oxygen and starts the IV while I draw 50 milligrams of diphenhydramine from a vial into a syringe. Diphenhydramine, better known by the trade name Benadryl, is one of the drugs we use to treat allergic reactions. With the IV set, her vitals signs checked, and oxygen being delivered through a nasal cannula, Sarah is ready to go. I push the Benadryl through the IV line, and we are on our way. The drug works quickly. Sarah feels the itching subside before we arrive at Rhode Island Hospital. So do I.
The midmorning rush is on at the ER. Seven rescues are parked in the cramped space, yet Mike manages to squeeze into the spot closest to the door. He shuts down the engine, gets out of the driver’s seat, and opens the rear door, letting the bright sunshine filter in. Sarah is much better; the Benadryl has helped. She tries again to escape the clutches of the ER by claiming that she is fine. I almost relent but in the end wheel her through the ER doors so they can treat her. There isn’t much that the ER staff can do now that the Benadryl has been administered and is working. She will have to wait for a few hours while they keep an eye on her airway. Sometimes when the drug wears off, the symptoms return, and airways close incredibly fast during an allergic reaction. I’ve seen patients breathing one minute, their airway completely blocked the next. It is a tragedy that happens all too often, frequently to the young and healthy.
A police officer working a detail at a local festival was stung by a bee one beautiful day last summer. He wasn’t aware of his bee sting allergy because he had never been stung. He ignored his symptoms as his heart rate increased, his hands began to swell, and hives erupted. His airway closed quickly, he fell to the ground gasping for a breath of the same air the festival-goers surrounding him breathed with ease. He was 37 years old and left a wife and a couple of kids.
The hospital is the best place for Sarah until the situation clears up.
The patients are stacking up, almost out the door. I see a few regulars; Darryl, wearing his old clothes and a stupid grin, is being escorted off the property by security. He will be back by noon, depending on how quickly he sells his stolen papers.
Rescue 5 backs into the bay before we leave, taking one of the spots just vacated. Rescues come and go all day. When their truck stops, I open the rear doors to say hello. Teresa is in back with another regular, this one a creepy homeless guy who claims to have chest pains a few times a week. He enjoys getting stuck with needles. He knows all the women on rescue by name, which I find disturbing. Teresa can’t help being nice to everybody she comes in contact with, and I hate seeing people like this guy take advantage of that kindness. Teresa is more than capable of handling herself, and this is her patient, so I let it rest.
I sometimes think it is my responsibility to look out for the new people on the other rescues. Most of the senior, experienced rescue officers are burned out by the sheer volume of calls and have left the division to join the firefighting force. Junior people, fresh out of the training academy, have been forced to fill the vacancies, most with a lot of EMT training but very little street experience. Some of them have only six months on the job. Rookies in Providence are in charge of some of the busiest rescues in the country. These “kids” have proven themselves time and time again. They have been exposed to horrors most people will never experience, have performed admirably—in some cases heroi - cally—and continue to do the job better than anybody has the right to expect.
“Hey, Teresa, how are you?” I ask while helping her move the “patient,” a 300-pound hypochondriac. I’m always happy to see Teresa. Her charm and attitude are contagious.
“Dude, what’s up?” she responds, her smile lighting up the back of the dingy rescue. She looks and sounds more like a California surfer girl than a firefighter in Providence.
“I think we’re getting breakfast. I’m sure Mike is due for his hourly feeding,” I say.
“Where are you going? We’ll meet you,” she replies while we wheel the patient from the rescue’s rear doors.
“Brook Street for some Mexican bagels,” I say.
There is a bagel shop across the street from the Brook Street fire station run by Mexican people who make the best bagels in the city. They also make breakfast burritos and nachos, but their bagels are what keeps me coming back.
“We’ll meet you there!”
Her partner, Tim, eats as much as Mike, and the three of them never gain a pound. There is a calendar in Rhode Island featuring “buff ” firefighters. Both Tim and Mike have graced the pages. I could too if I wanted—if I weren’t old, fat, and ugly.
Tim and Teresa take their patient into the ER, and Mike and I head for the bagel store. I put us at the mercy of the dispatchers when I key the mike and go in service. The chances of us actually meeting Tim and Teresa for breakfast are slim, but we try to make the job a little more enjoyable.
“Where are you going?” I ask Mike as he turns the truck away from the Brook Street bagel store.
“Dunkin’ Donuts,” he replies matter of factly.
“We’re going to Brook Street,” I said, asserting my rank.
“You always get two bagels when we go there,” Mike replies, not impressed.
“I want two bagels.”
“If you quit complaining about how fat you’re getting, we would go to Brook Street.”
“If you mind your own business, I won’t fire you!”
“Fire away,” he says while laughing hysterically. “I need the time off.”
I have to laugh as well.
Mike stops in front of the Dunkin’ Donut shop and says, “What do you want? I’m buying.”
“You bought yesterday; I’ve got it. The usual?” I ask.
“No, just a coffee. Art made pancakes while you were sleeping.”
“Why didn’t you wake me up?”
“You would have killed me.”
“Now I’m really going to kill you!” I love pancakes.
I cross Eddy Street and wait in line. I get only one bagel and Mike’s coffee. “What time does Venda open?” I ask Mike while handing him his drink.
“They’re open now. Do you want to head over there?”
We have a lot to do today between runs, including refueling the truck and going to the repair shop to fix a thing that holds the stretcher in place. Rescue 1 is less than a year old but is already showing signs of wear and tear. We also have to go to a medical oxygen supply depot. The truck is equipped with a large O2 tank that lasts a couple of weeks and some smaller portable tanks, and all are almost empty.
“Nah, let’s go back to quarters and get the maintenance out of the way. We’ll go this afternoon,” I say.
“You’re going to forget.”
“Never happen.”
Mike asks, “Why do you eat manicotti on Easter anyway? What’s wrong with ham?”
“It’s an Italian thing,” I explain. “There’ll be plenty of ham and all that, but Cheryl and the girls like pasta, so we always get something to go with the gravy.”
“Giving the girls what they want—smart man,” Mike says as we head toward the station.
Fire stations and the apparatuses they hold don’t take care of themselves. Back at the barn, spring cleaning is under way Captain Healy is a true taskmaster at this time of year. He learned how to clean a fire station from the volunteer firefighters in his hometown, Warren, Rhode Island, and hasn’t changed a thing. Hot water, soap, and elbow grease are all that matter to him during spring cleaning. He posted a cleaning list on the bulletin board a few weeks ago and expected the work to be done in an expeditious manner. Each group is responsible for a section of the station, with the captain of the house designating the assignments. Having the captain on our shift should have been a good thing, but Captain Healy marches to the beat of his own drummer. He decided to give us most of the work “to be fair.”
Rescue 1 is responsible for the apparatus floor bathroom and two of the offices in the living quarters. Mike will take care of the bathroom while I start to do the offices. Whether or not we finished our tasks is up to the rescue gods. When we need them to chime in, they never do. I fill a bucket with hot, soapy water and begin to clean.
Downstairs, I hear all hell breaking loose. Shouts and hysterical laughter are coming through the holes in the floor where the sliding poles are. Being a cagey old veteran, I know this can only mean one thing: water fight! No respectable spring cleaning would be complete without one.
Mike is outnumbered. I know that the guys from Engine 13 are ganging up on him. Nothing is fair when it comes to water fights. The only rule is “There are no rules!” Too bad for Engine 13, they have forgotten that I am upstairs and have years of water fight experience. I fill three big pans with water and place them on a windowsill in the dorm, directly over Engine 13’s overhead door. I leave the weapons on the ledge and retreat to my locker.
Inside is a package of water balloons left over from last year. I fill four of them from the sink in the kitchen. Once through, I booby-trap the kitchen sprayer by holding it open with a rubber band wrapped around the handle. In the bathroom, I point the showerheads directly in the path of whoever will turn the lever. I strategically place the balloons on the top landing of the stairs. I am ready to join the battle.
I am the only one on the upper level and can use that to my advantage. The guys from Engine 13 are on the ramp, buckets of water or hoses in hand, waiting to ambush Mike. Captain Healy, a cagey veteran himself, is nowhere to be seen, but I can’t worry about him just now. If I can quietly open the window above them, I’d have a clean shot. If they hear me, I’m as good as dead. I can only see two of them, which leaves the other two unaccounted for. Not good. The potential for surround-and-drown tactics from the enemy is growing as each valuable second ticks.
This is a battle I hadn’t anticipated. Without proper communication with Mike, the success of the entire operation is in jeopardy. We have never been to war together, but I hope his instincts will see us through. I gently push the window up, but it hasn’t been opened since the fall and gets stuck. I feel my heart pounding out of my chest and hope the enemy can’t hear it thumping. Sweat pours down my forehead and into my eyes, blinding me. The window finally gives, but not without a loud “crack!” I jump from my position, and, as the targets look up, I unload with everything I have.
Direct hit!
My first mission accomplished, I run to the top of the stairs to head off the counterattack. If my calculations are correct, Mike will flank them from behind, brandishing the hose we use to wash the trucks. I should make it to the landing in time to retrieve the water grenades and we’ll have them in crossfire. I leave my position and head for the stairs.
“Engine 13 and Rescue 1, a still alarm.”
War is hell. My brilliant plan would have to wait. I abort the mission and head for the truck. An uneasy truce has been declared.


